Research news
New tool to visualize the toxic protein responsible for Huntington’s disease
Huntington’s disease (HD) is an incurable neurological disorder caused by a genetic mutation in the DNA of a specific gene called huntingtin. An inherited mistake in the huntingtin gene generates a toxic misfolded protein, defined as mutant huntingtin (mHTT). Accumulation of this protein damages the cells in the brain, leading to symptoms such as uncontrolled movements and cognitive disorders.
A major goal of researchers is to investigate whether stopping or reducing the rate of accumulation of mHTT could be an effective treatment for HD. However, to understand whether therapy is effectively slowing down the accumulation of toxic mHTT, we need to be able to measure the toxic mHTT responsible for the disease. In a study published in the prestigious scientific journal Science Translational Medicine, researchers from the University of Antwerp and their collaborators described a new tool to see and quantify the toxic aggregated mHTT protein in the living brain.
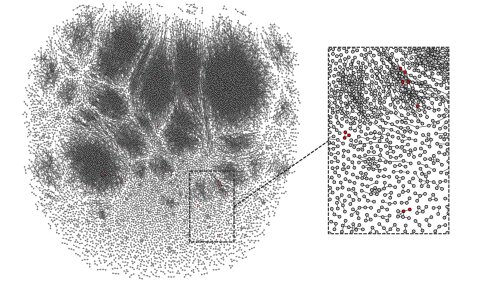
Dr. Bertoglio and colleagues developed a new imaging tool to visualize the toxic aggregated mHTT protein. “Using this non-invasive imaging technique, we could observe and measure the amount of harmful mHTT accumulating in the brain of mice with Huntington’s disease (Figure 1). In addition, we tested this imaging approach with novel therapies effective in reducing mHTT load. Mice with lower mHTT levels have reduced signal with this tool, suggesting this novel imaging method could be used to evaluate whether different types of therapies effectively reduce the toxic mHTT load in the brain.”
A next step will be to test this novel approach in patients with HD and evaluate whether HD and its treatment can also be monitored in humans with this imaging tool. “This unique method can prove crucial to helping scientists and doctors understand how the disease progresses in the different parts of the brain. Moreover, it has huge potential for understanding which potential treatments might be best for a given patient at a given time as well as how well treatments are working.”
Reference to the study: Bertoglio et al., Sci. Transl. Med. 14, eabm3682 (2022)
Pre-existing immune cells can predict early response to hepatitis B vaccine
Impact statement: Immunosequencing of T cells, combined with machine learning techniques, may enable scientists to predict which patients will have early, strong protection against hepatitis B infection following vaccination.
Cambridge, UK – 8am GMT / 9am CET / 3am EST, Tuesday, January 25, 2022
Researchers have shown how pre-existing immune cells in the blood may help individuals develop rapid and strong protection against hepatitis B infection following vaccination.
Their methods, described today in eLife, may lead to new ways for scientists and clinicians to predict which individuals will be protected by vaccination against hepatitis B infection, and who may have a delayed or inadequate immune response. It may also help them better understand how individuals develop natural immunity to pathogens or immunity following vaccination.
Immune cells called CD4 T cells help the body recognise pathogens. They also recognise vaccine antigens that help the body identify and develop immunity to the pathogens. Once a CD4 T cell recognises a pathogen or a vaccine antigen, it develops into a memory cell ready to defend the body quickly against future infections.
“Some people also have pre-existing memory CD4 T cells that recognise pathogens or vaccine antigens that they haven’t even been exposed to before. We wanted to find out if having pre-existing memory CD4 T cells that recognise the hepatitis B vaccine surface antigen helps individuals develop immunity after vaccination,” explains George Elias, who worked on the study while he was a PhD student at the Vaccine and Infectious Disease Institute, University of Antwerp, Belgium. Elias is a co-first author of the study alongside Pieter Meysman and Esther Bartholomeus (University of Antwerp).
To answer this question, the team recruited 34 people who had never been exposed to hepatitis B or vaccinated against it. They collected blood samples from these individuals before and after they were given two doses of the hepatitis B vaccine. They then used next-generation sequencing and machine learning methods to analyse the memory CD4 T cells in these individuals before vaccination and at three time points following vaccination.
Their analysis revealed that participants with a higher number of pre-existing memory CD4 T cells that recognised the vaccine antigen developed immunity more quickly and produced more antibodies following vaccination. They also showed that using immunosequencing to analyse the participants’ pre-existing memory CD4 T cells could predict whether they would rapidly produce strong immunity after hepatitis B vaccination.
The authors say that the ability of CD4 T cells to recognise multiple antigens may explain why even people who have never been exposed to hepatitis B or its vaccine have pre-existing memory cells that recognise the virus. These memory cells may have been generated in response to environmental exposures or to microbes that live in the human body, but more research is needed to better understand their origins.
“Our analysis has uncovered a role for pre-existing memory CD4 T cells in mounting a quick and powerful immune response to the hepatitis B vaccine,” concludes Benson Ogunjimi, Co-Founder and Biomedical Coordinator of the Antwerp Unit for Data Analysis and Computation in Immunology and Sequencing (AUDACIS), and a co-senior author of the study alongside Viggo Van Tendeloo and Kris Laukens (AUDACIS). “We’ve shown that pre-existing memory CD4 T cells could affect the outcome of vaccination, which may have significant implications for immunity and vaccine development efforts.”
Ogunjimi and his co-authors have launched a company based on the next-generation sequencing methods described in their work. ImmuneWatch works to provide in-depth sequencing and analysis of the human T-cell response, and aims to transform this data into clinically actionable insights for the development of improved vaccines and immune therapies.
More information about ImmuneWatch is available at https://www.immunewatch.com.
Author contacts:
Benson Ogunjimi, Co-Founder and Biomedical Coordinator
Vaccine and Infectious Disease Institute, University of Antwerp
Antwerp Unit for Data Analysis and Computation in Immunology and Sequencing, University of Antwerp
Pieter Meysman, Postdoctoral Researcher and Startup CTO
Adrem Data Lab, University of Antwerp
Antwerp Unit for Data Analysis and Computation in Immunology and Sequencing, University of Antwerp
Kris Laukens, Co-Founder and Scientific Advisor
Adrem Data Lab, University of Antwerp
Antwerp Unit for Data Analysis and Computation in Immunology and Sequencing, University of Antwerp
About eLife
eLife is a non-profit organisation created by funders and led by researchers. Our mission is to accelerate discovery by operating a platform for research communication that encourages and recognises the most responsible behaviours. We review selected preprints in all areas of biology and medicine, including Immunology and Inflammation, and Microbiology and Infectious Disease, while exploring new ways to improve how research is assessed and published. eLife receives financial support and strategic guidance from the Howard Hughes Medical Institute, the Knut and Alice Wallenberg Foundation, the Max Planck Society and Wellcome. Learn more at https://elifesciences.org/about.
To read the latest Immunology and Inflammation research published in eLife, visit https://elifesciences.org/subjects/immunology-inflammation.
And for the latest in Microbiology and Infectious Disease, see https://elifesciences.org/subjects/microbiology-infectious-disease.