By: Jill Meirte, MOVANT Research Group, Department of Rehabilitation Sciences and Physiotherapy (REVAKI), University of Antwerp, Wilrijk, Belgium; Oscare, a research and aftercare centre for patients with scars and burns, www.oscare.be, Antwerp, Belgium
Introduction
Surgery is a common and often necessary procedure for individuals diagnosed with cancer. While advancements have made surgeries less invasive, patients still face potential complications such as hypertrophic scarring and scar adhesion1. Sometimes, in addition, post-treatment with radiotherapy adversely affects fibrosis of skin and scar tissues 2. Although post-surgical scars are often not considered a top priority at the time of occurrence, hypertrophic or pathological scars have been shown to have a major impact on the patient's/their quality of life 3,4. The follow-up of these scars and their impact on the patient after surgery is important but is not done systematically in clinical practice. There is a need for better postoperative scar follow-up. Moreover, it is possible to prevent the process of hypertrophic scarring after surgery.
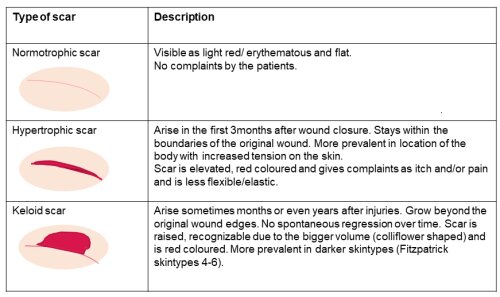
Understanding Post-surgical Scars
Wounds resulting from burns, trauma, or surgery undergo a natural healing process, forming new skin. Unfortunately, this repair process can lead to pathological scars, characterized by excessive proliferation of skin tissue and collagen deposition5. Scar maturation takes time, with scars evolving from immature to mature over two to five years6. Hypertrophic and keloid scars are common post-surgical outcomes, each with distinct physical characteristics and associated symptoms. Hypertrophic scars, occurring in 30% to 50% of cases9, manifest as raised, red, and painful scars within the boundaries of the original wound. Timely prevention and follow-up during the initial three months post-surgery are crucial (see Table 1).
Reported Characteristics and Symptoms
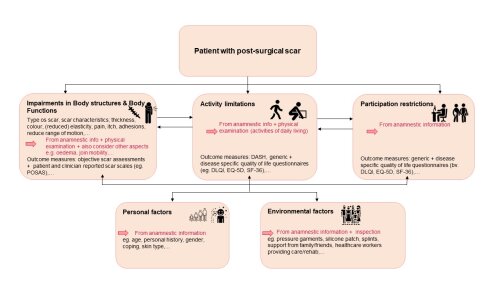
Even with the evolution of less invasive surgical techniques, patients undergoing cancer surgery may experience mental, physical, and social impacts1. The International Classification of Functioning, Disability, and Health (ICF) framework created by the WHO provides a holistic approach to evaluating the multifaceted consequences of hypertrophic scars10. These consequences include aesthetic concerns, long-term impairments in anatomical features and functions, leading to activity limitations and participation restrictions. Utilizing standardized questionnaires such as the Patient and Observer Scar Assessment Scale (POSAS) and the Dermatology Life Quality Index (DLQI) aids in assessing the impact on the patient's quality of life. Holistic follow-up involves considering a range of parameters and outcome measures to comprehensively evaluate the patient's experience (see Figure 1).
Anamnestic and Clinical Examination
Comprehensive patient assessment involves a detailed interview and thorough physical examination, including scar palpation. Factors like delayed wound healing and scar location can influence hypertrophic scarring development. Standardized questionnaires, like the Patient and Observer Scar Assessment Scale (POSAS)11 and the Dermatology Life Quality Index (DLQI) 12, enhance the assessment of scar quality and its impact on the patient’s quality of life. These questionnaires have been validated, take only a few minutes to administer and are convenient for clinical practice as they can be used in all types of scar patients and together map important aspects ICF wide4. We know from research that the use of questionnaires increases patient engagement, helps identify unique needs and contributes to patient-centered clinical decision-making.13 Continuity of care, teaching patients how to self-care for scars and psychosocial follow-up appear to be important contributors to patient-centered scar follow-up. During the care process, going through the completed scales together can help with the holistic view of scar progression and help inexperienced patients understand their scar symptoms14. Patient engagement, continuity of care, and psychosocial follow-up are vital contributors to patient-centered scar follow-up.
Figure 1: ICF form with overview of relevant aspects of ICF-domains to evaluate in patients with (post-surgical) scars, together with relevant outcome measures.
Preventive and Curative Practical Guidelines
Preventive measures for linear scar treatment encompass good wound care, hydration, sun protection, silicone application, pressure therapy and tension-reducing taping. Curative guidelines include scar massage, silicone therapy, pressure therapy, taping, and hydration15. While various non-invasive treatment options exist, pressure therapy and silicone therapy have the most evidence for preventing and treating hypertrophic scars 16, 17.
Recommendations
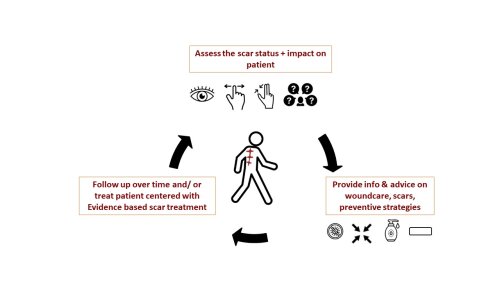
Post-surgical scars can significantly impact a patient's quality of life after oncological surgery. A patient-centered assessment using the ICF framework and validated questionnaires is essential to develop individualized treatment plans. Incorporating quality of life questionnaires and scar scales throughout the care process ensures a holistic evaluation, considering the patient's perspective. Inclusion of patient values, goals, and preferences in the treatment plan promotes individualized care. Ongoing communication and collaboration enhance trust and patient satisfaction. Providing information and specific attention to post-surgical scars minimizes their impact on daily lives (see Figure 2).
Figure 2: Illustration depicting the holistic approach to post-surgical scar management.