Why frozen shoulder should already be treated in the early phase

Frozen shoulder is a debilitating and annoying disorder and this may be an understatement. Frequently, in the early stage, general practitioners and specialists do not recommend treatment, because of the debilitating pain and inappropriate applied interventions. Additionally, it was thought for many years that frozen shoulder would resolve by time without treatment. Therefore, frozen shoulder is referred to as a self-limiting disorder.
Unfortunately, there were several patients who did not recover completely and some even held severe pain.1 A few years ago evidence arose that this self-limiting character is not true and it appears to be difficult to investigate the true self-limiting character of frozen shoulder.2 Anyway, this evidence suggests that there is rather a fast and early recovery that slows with time, which is contrary to the original idea that recovery takes place in the later phases of the disorder. With our frozen shoulder research project, we can confirm the presence of a rather fast recovery that slows with time, which is independent of treatment. Therefore, it seems important to start rehabilitation as soon as possible after diagnosing frozen shoulder.
Regrettably, the optimal treatment for frozen shoulder is still unknown.3 Nevertheless, there are some guidelines available for the rehabilitation of frozen shoulder.4, 5 These guidelines suggest to use tissue irritability to guide treatment. This is a very useful strategy to help patients with frozen shoulder recover from their symptoms and return to their pre-injury work and sports level.
From these irritability levels, I want to focus on the high irritability level and progress towards moderate irritability. In the high irritability level, patients experience a high level of pain, they have frequent night and/or rest pain, they experience pain during the complete movement trajectory and the active range of motion is usually smaller than the passive range of motion. These complaints are probably the consequence of an active inflammatory process.
Pain is one of the most annoying complaints in the high irritability level. You might have read about the pain-monitoring model in the blog post of Claudia Cavaggion (Provoke pain to get rid of it?). In this model, a pain score up to 5 is acceptable after exercises. It is even proposed to go into pain during rehabilitation, which might have larger benefits in certain cases. However, for patients with frozen shoulder in the high irritability level, it is important to stay in the pain free range. Provoking pain in these patients will increase the range of motion restriction and increase the complaints. Why does this happen in patients with frozen shoulder?
Inflammation results in proliferation, activation and differentiation of fibroblasts and collagen synthesis might be dysregulated.6{Kraal, 2020 #8685}{Kraal, 2020 #8685} Persistent activation of fibroblasts enhances the inflammatory response and is a potential mechanism of symptoms of prolonged stiffness.6Myofibroblasts are cells involved in the inflammatory process after injury. There is some inconsistency in the results regarding the presence of myofibroblasts in the area of the rotator interval of the shoulder joint capsule. However, the presence of myofibroblasts in the early phase (high irritability) of frozen shoulder explains the adverse reaction and increased pain to passive mobilization and capsular stretching in this phase. Greater stress, as occurs during passive mobilization and capsular stretching, will contract these myofibroblasts more and they enhance the inflammatory response.
Based on this knowledge, you can imagine that rehabilitation in the high irritability phase should focus more on advising and guiding these patients:
· Inform the patient about the disease frozen shoulder (despite there is still a lot of debate about it);
· Provide them answers to the 5 questions of the common sense model (What is it? What is the cause? How long will it take? What can I do about it? What are the consequences?);7
· Cooperate with other healthcare providers to offer the same message to the patient;
· Involve all people who are part of the social environment to increase treatment adherence;
When healthcare providers offer different information, this might confuse patients and result in detrimental and negative stress, inhibiting the recovery process. Additionally, pharmacotherapy can be beneficial in reducing pain. When the pain is even worse and untenable, a corticosteroid injection by a shoulder specialist can be considered. In this phase, active or active assisted low intensive mobilizations and various types of exercises are allowed, as long as it is pain free. This can be done under the supervision of a physical therapist.
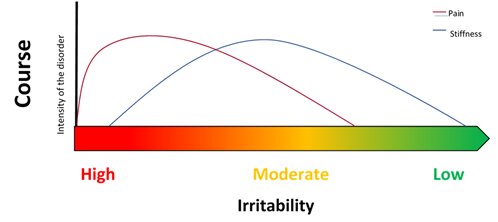
When the patient is progressed to a moderate irritability, patients usually have a moderate pain level, only occasionally night and/or rest pain, experience pain in the end position of active and passive movements and active and passive range of motion are similar. These improving complaints probably indicate a decreased inflammatory activity. Consequently, rehabilitation can be intensified.
In this irritability level, rehabilitation can progress more towards end range. A healthcare provided can carefully introduce passive mobilization and increase the intensity of exercises. Furthermore, patients can reintegrate more daily activities in their recovery and a maximum of 4 hours of tissue response is acceptable now.
If you want to read more about effective and potential new conservative interventions you can read our review: “An overview of effective and potential new conservative interventions in patients with frozen shoulder”.8 If you are interested in new updates regarding frozen shoulder, keep an eye on the Social Media of MOVANT or follow me on twitter (@michelmertens4) or LinkedIn (Michel Mertens). Of course, you can also send me an e-mail if you have specific questions: Michel.mertens@uantwerpen.be.
Researcher international research group Pain in Motion (http://www.paininmotion.be/)
2021 MOVANT research
Further reading:
1. Hand C, Clipsham K, Rees JL, et al. Long-term outcome of frozen shoulder. J Shoulder Elbow Surg 2008; 17: 231-236. 2007/11/13. DOI: 10.1016/j.jse.2007.05.009.
2. Wong CK, Levine WN, Deo K, et al. Natural history of frozen shoulder: fact or fiction? A systematic review. Physiotherapy 2017; 103: 40-47. 2016/09/20. DOI: 10.1016/j.physio.2016.05.009.
3. Forsythe B, Lavoie-Gagne O, Patel BH, et al. Efficacy of Arthroscopic Surgery in the Management of Adhesive Capsulitis: A Systematic Review and Network Meta-analysis of Randomized Controlled Trials. Arthroscopy 2021; 37: 2281-2297. 20201120. DOI: 10.1016/j.arthro.2020.09.041.
4. Vermeulen H, Schuitemaker R, Hekman K, et al. De SNN Praktijkrichtlijn Frozen Shoulder voor fysiotherapeuten 2017. maart 2017 2017.
5. Kelley MJ, Shaffer MA, Kuhn JE, et al. Shoulder pain and mobility deficits: adhesive capsulitis. J Orthop Sports Phys Ther 2013; 43: A1-31. 2013/05/03. DOI: 10.2519/jospt.2013.0302.
6. Kraal T, Lübbers J, van den Bekerom MPJ, et al. The puzzling pathophysiology of frozen shoulders - a scoping review. J Exp Orthop 2020; 7: 91. 2020/11/19. DOI: 10.1186/s40634-020-00307-w.
7. Leventhal H, Brissette I and Leventhal E. The common-sense model of self-regulation of health & illness. The self-regulation of health & illness behaviour. London: Routledge Taylor & Francis Group, 2003, pp.42-60.
8. Mertens MG, Meeus M, Verborgt O, et al. An overview of effective and potential new conservative interventions in patients with frozen shoulder. Rheumatol Int 2021 2021/09/07. DOI: 10.1007/s00296-021-04979-0.